Views: 0 Author: Site Editor Publish Time: 2025-12-17 Origin: Site








Healthcare workers operate in one of the most physically demanding environments imaginable. Yet, paradoxically, one of the simplest tools supporting their work—a proper chair—is often deprioritized, neglected, and chronically absent from clinical units. This isn't merely a comfort issue; it's a workplace safety crisis with cascading consequences for staff retention, patient safety, and operational efficiency.

As healthcare furniture specialists, we've witnessed countless healthcare facilities grapple with the same recurring problem: staff seating shortages that force nurses and clinical workers into corridor charting, compromised infection control, and preventable occupational injuries. This comprehensive guide provides evidence-backed solutions grounded in real-world case studies and professional standards.
The staff chair shortage in healthcare facilities is not anecdotal—it's systemic. Consider these testimonials from frontline healthcare workers:
"We have roughly 13 chairs for staff to utilize while charting. 12 of the 13 have some defect or are unusable. Four new chairs were bought for the doctor's dictation room..."
This statement encapsulates a core problem: prioritization bias favoring physician spaces over nursing stations. When healthcare administrators allocate furniture budgets, clerical and administrative areas frequently receive new seating while clinical nursing units deteriorate.
1. Inadequate Quantity Creating Workflow Chaos
Staff are forced to:
Roll computers and chairs into hallways and side areas to chart
Share limited seating, creating scheduling conflicts during shift changes
Stand for extended periods while documenting patient care
Rotate chairs between units, disrupting workflow continuity
2. Damaged Furniture Beyond Safe Use
Existing chairs exhibit:
Torn upholstery with stuffing protruding
Exposed nails and metal edges
Weakened frames unable to support full body weight
Seat cushions with insufficient support
3. Infection Control Compromises
Damaged seating creates:
Crevices where bacteria and pathogens accumulate
Difficulty cleaning and disinfecting
Increased infection transmission risk
Non-compliance with healthcare facility standards
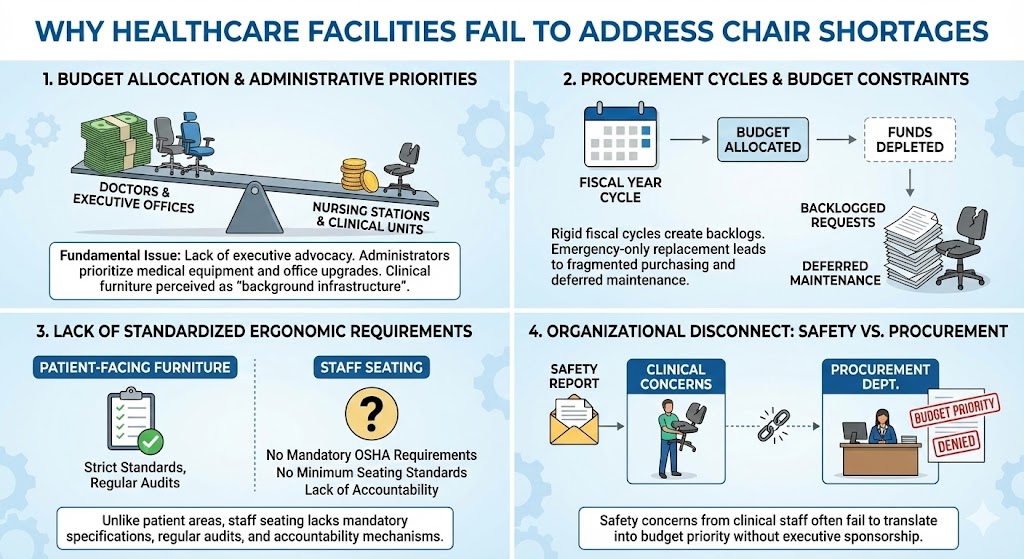
The Fundamental Issue: Nursing stations lack executive-level advocacy compared to medical offices.
Administrators observe:
Doctors and executive staff directly request office furniture upgrades
Nursing departments submit less visible needs
Clinical unit furniture is perceived as "background infrastructure"
Budget committees prioritize new medical equipment over staff ergonomics
The Irony: Investing in staff seating yields measurable ROI through reduced worker injuries and improved retention—yet remains undervalued in capital planning discussions.
Healthcare facility budgets operate on rigid fiscal year cycles. Once allocated, they're depleted. Staff chair replacement often doesn't align with budget timelines, creating:
Multi-year backlogs of equipment requests
Emergency-only replacement (when chairs become safety hazards)
Fragmented purchasing that prevents standardized solutions
Deferred maintenance on existing inventory
Unlike patient-facing furniture governed by strict standards, staff seating lacks:
Mandatory OSHA requirements for quantity and ergonomic specifications
Facility standards mandating minimum seating per unit
Regular audits of staff workspace functionality
Accountability mechanisms for chair procurement delays
One healthcare professional's experience illustrates this disconnect:
"I sent a thorough email detailing the specific problems with each chair, highlighting staff concerns, OSHA standards, and providing potential chair options along with their prices. [Management response was minimal]"
The Problem: Safety concerns raised through formal channels don't translate into budget priority without executive sponsorship. Procurement departments lack direct feedback on the clinical impact of inadequate seating.
Research Finding: According to the Cal/OSHA Safe Patient Handling Regulation framework, workplace ergonomic hazards directly contribute to healthcare worker injuries. When healthcare facilities implement comprehensive ergonomic workstation improvements—including proper seating—injury rates demonstrate measurable improvement.
Baseline Statistics: Healthcare workers experience musculoskeletal disorder rates 3-4 times higher than manufacturing workers
Ergonomic Intervention Impact: Facilities implementing comprehensive ergonomic upgrades (including staff seating) report 20-35% reductions in back injuries and strain-related claims
Cost Savings: Each prevented back injury saves healthcare facilities $10,000-$30,000 in direct medical costs and lost productivity
Why This Matters: One serious back injury from poor seating ergonomics costs more than 5-10 years of proper chair maintenance and replacement cycles.
Research Finding: The HCD Expo 2025 industry survey revealed that ergonomic workspaces—particularly proper seating—rank in the top three factors affecting healthcare worker retention decisions.
Turnover Cost: Replacing a single registered nurse costs 0.75-1.5x annual salary ($55,000-$85,000 for average RN salary)
Seating Impact: Healthcare workers cite "lack of basic working conditions" (including inadequate seating) as primary reasons for career exits
Staff Satisfaction Correlation: Facilities with comprehensive ergonomic staff workstations report 15-25% improvement in retention metrics
Why This Matters: A single prevented nursing vacancy pays for 200-400 ergonomic staff chairs, yet chair investment remains underfunded.
Research Finding: Damaged, porous furniture surfaces harbor pathogenic bacteria and complicate infection control protocols. According to healthcare facility infection prevention standards, seating damaged beyond routine cleaning represents a compliance violation.
Compliance Risk: Facilities with deteriorated staff furniture face regulatory scrutiny and accreditation challenges
Replacement Cost: Emergency furniture replacement (driven by compliance failures) costs 40-60% more than planned replacement cycles
Operational Impact: Damaged seating restricts charting locations, creating bottlenecks and workflow inefficiencies that indirectly delay patient care
Why This Matters: Proactive chair replacement prevents costlier compliance remediation and avoids operational disruptions.
One frustrated healthcare worker captured the underlying issue:
"Our staff roll computers and chairs into a side hall to chart...I told admin I was not addressing that issue until they gave my nurses a place to go."
And the ultimate illustration of how problems get solved:
"I had to steal four chairs from the offices and wheel them up to the unit. Guess who had all new chairs within a week!"
This is the tragic conclusion: Staff must take matters into their own hands through informal reallocation because formal channels fail to deliver. When visible chair shortages embarrass administration, only then do resources flow.
This reflects a systemic failure where working conditions aren't prioritized until they become visible crises.
Addressing healthcare worker chair shortage requires solutions across four interconnected domains: procurement strategy, ergonomic standards, organizational governance, and facility-wide implementation.
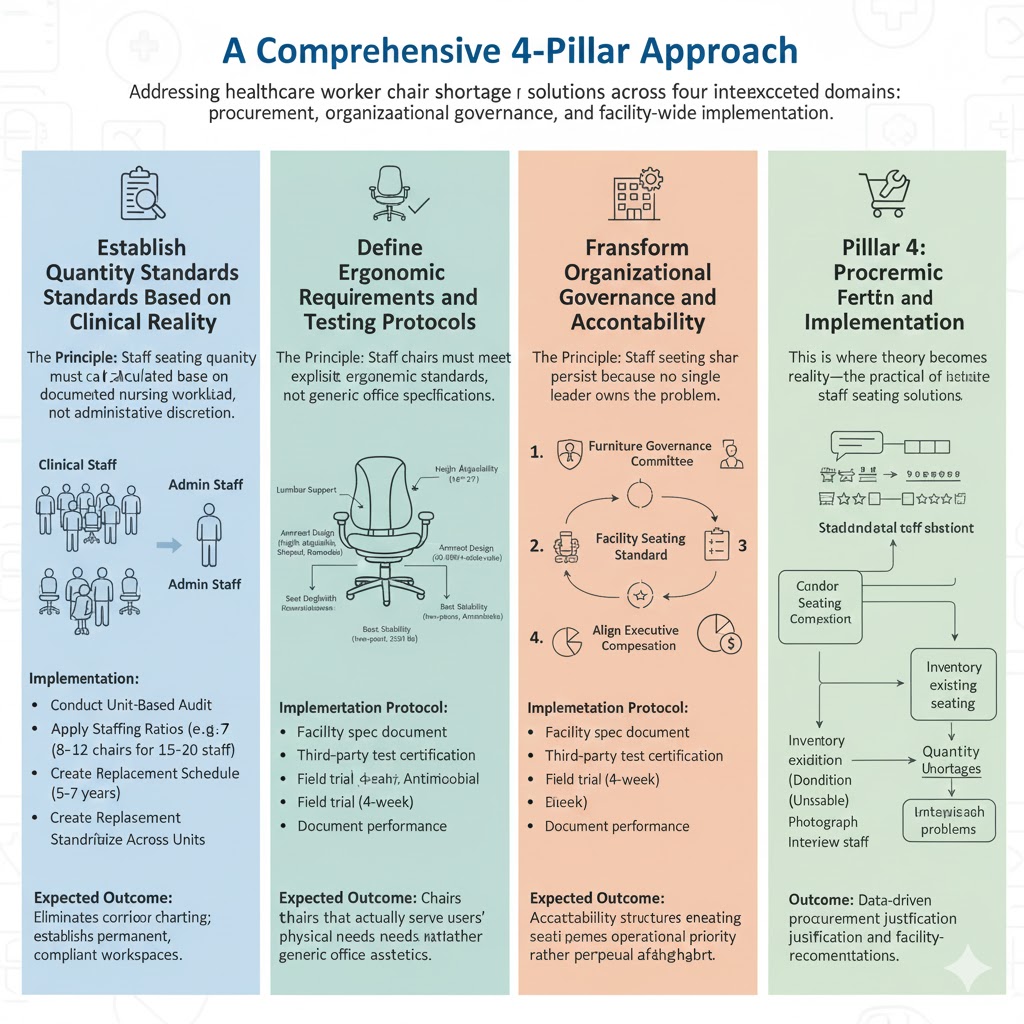
The Principle: Staff seating quantity must be calculated based on documented nursing workload, not administrative discretion.
Implementation:
Conduct Unit-Based Audit: Count active staff during peak and low-census periods; document current charting locations
Apply Staffing Ratios: Healthcare facilities operating with 15-20 clinical staff per unit should have minimum 8-12 dedicated staff chairs (accounting for simultaneous charting, breaks, and equipment use)
Create Replacement Schedule: Establish rotating furniture replacement every 5-7 years to prevent sudden deterioration
Standardize Across Units: Implement facility-wide baseline standards rather than unit-by-unit variation
Expected Outcome: Eliminates corridor charting; establishes permanent, compliant workspaces.
The Principle: Staff chairs must meet explicit ergonomic standards, not generic office specifications.
Key Ergonomic Requirements for Healthcare Nursing Station Chairs:
1. Height Adjustability: Chairs must accommodate 5th percentile to 95th percentile user populations with adjustable seat height (16"-21" range minimum)
2. Lumbar Support: Integrated or adjustable lumbar support reducing lower back strain during 8-12 hour shifts; independent support adjustment for diverse body types
3. Armrest Design:
Height adjustable (18"-22" range) for proper shoulder positioning
Shaped to prevent cubital tunnel compression on forearms
Removable or flip-up design for flexible workstation integration
4. Seat Depth and Width:
Seat depth 16"-18" preventing hyperflexion of knees
Sufficient width (18"-20") for comfort without excessive lateral movement
5. Material Durability:
Heavy-duty upholstery withstanding 150,000+ double-rubs (ASTM D4157 test standard)
Moisture-resistant, stain-resistant performance fabrics
Seamless construction minimizing crevices where pathogens accumulate
6. Base Stability:
Five-point base preventing tip-over under standard use
Smooth-rolling casters appropriate for healthcare flooring
Weight capacity minimum 250 lbs
7. Cleanability:
Non-porous seat surfaces enabling rapid disinfection
Removable cushion covers (where applicable)
Hospital-grade antimicrobial fabric options
Implementation Protocol:
Establish facility furniture specification document requiring these criteria
Require manufacturers provide third-party test certification
Conduct field trial (4-week minimum) with end-user feedback before full procurement
Document performance metrics during trial period
Expected Outcome: Chairs that actually serve users' physical needs rather than generic office aesthetics.
The Principle: Staff seating shortages persist because no single leader owns the problem.
Structural Changes Required:
1. Establish a Furniture Governance Committee
Members: Chief Nursing Officer, Environmental Services Director, Occupational Health & Safety Manager, Frontline Nurse Representative, Procurement Director
Quarterly Meetings: Review facility seating inventory, replacement timelines, and staff feedback
Authority: Committee recommendations bypass standard approval hierarchies for urgent seating needs
2. Create a Facility Seating Standard
Establish minimum chairs per unit type (ICU, Medical-Surgical, Emergency, Specialty)
Define replacement cycle (5-7 years) built into annual budgets as fixed costs
Require Environmental Services quarterly audits documenting chair condition
3. Implement Staff Feedback Mechanisms
Anonymous survey tools assessing seating adequacy and ergonomic problems
Rapid response protocol when staff report damaged chairs (48-hour evaluation, 5-day maximum repair/replacement)
Direct escalation pathway when seating problems impact patient care workflows
4. Align Executive Compensation with Staff Working Conditions
Include "staff ergonomic workspace adequacy" metrics in C-suite performance evaluations
Tie department budgets to compliance with seating standards
Make staff satisfaction metrics visible to hospital boards
Expected Outcome: Accountability structures ensuring seating becomes operational priority rather than perpetual afterthought.
This is where theory becomes reality—the practical execution of healthcare staff seating solutions.
Before purchasing a single chair, understand current state:
Inventory all existing staff seating across all units
Document condition (fully functional, damaged-minor, damaged-major, unusable)
Document quantity shortages per unit
Photograph specific problems (torn upholstery, broken frames, etc.)
Interview staff regarding ergonomic problems
Outcome: Data-driven procurement justification and facility-specific recommendations.
Not all furniture vendors understand healthcare's unique demands. Partner with manufacturers possessing:
Documented Healthcare Experience: Track record of major medical facility projects
Customization Capability: Ability to adapt designs to facility-specific workflows
Durability Standards: Products tested and proven in high-use healthcare environments
Compliance Knowledge: Understanding of infection control, OSHA, and regulatory requirements
Support Infrastructure: Warranty, repair services, and replacement logistics
Case Study: Hongye Furniture's Saudi German Hospital Makkah Medical Project
The Saudi German Hospital Makkah Medical Project Solution by Hongye Furniture exemplifies this approach. This comprehensive medical furniture project demonstrates how specialized manufacturers address healthcare facility needs:
Project Scope:
Customized furniture solutions for a major Saudi Arabian medical facility
Integration of medical equipment requirements with ergonomic staff workspaces
Precision engineering accounting for facility-specific architectural constraints
Complete project coordination from design through installation




Saudi German Hospital Makkah | Medical Project Solution By Hongye Furniture
Key Advantages Demonstrated:
1. Specialized Expertise: Hongye brought 30+ years of healthcare furniture experience, understanding the specific demands of Middle Eastern medical facilities
2. Customization: Rather than standard off-the-shelf seating, solutions were tailored to the hospital's workflow, space constraints, and regulatory environment
3. Quality Assurance: Documented durability testing ensuring furniture withstands rigorous healthcare use
4. Project Management: Coordinated logistics, installation, and quality verification across complex facility requirements
Lessons Applicable to Any Healthcare Facility:
Don't settle for generic office furniture: Medical facilities require specialized vendors
Customization matters: Off-the-shelf solutions often fail to address facility-specific workflow issues
Integrated approach works: Treating staff seating as part of comprehensive facility design (rather than afterthought) produces superior outcomes
Manufacturer partnership: Long-term relationships with specialized providers enable ongoing support and optimization
This project illustrates that when healthcare facilities partner with experienced manufacturers understanding clinical workflows, the resulting seating solutions actually address frontline needs.


Black Leather Executive Modern Luxury Office Chair with Arms
Healthcare facilities that implement comprehensive staff seating solutions achieve measurable outcomes:
| Metric | Baseline | Post-Implementation | Timeline |
Staff-reported back pain/discomfort | 60-70% of nurses | 25-35% | 6-12 months |
Occupational injury claims (back/strain) | 8-12 per year (100+ bed facility) | 3-5 per year | 12-18 months |
Staff seating-related equipment downtime | 15-20 hours/month/unit | 1-2 hours/month/unit | Ongoing |
Nurse retention (facility-specific) | Regional baseline (average 85%) | 92-95% | 18-24 months |
Compliance audit findings (seating) | Multiple deficiencies | Zero deficiencies | 6-12 months |
Staff satisfaction (workspace adequacy) | 35-45% satisfaction | 85-90% satisfaction | 12-18 months |
Return on Investment: A 200-bed hospital implementing comprehensive staff seating improvements invests approximately $150,000-$200,000 in quality chairs. Within 24 months, prevented worker injuries and reduced turnover typically generate $300,000-$400,000 in measurable cost savings.
The most damaging impact of seating shortages isn't discomfort—it's operational dysfunction. When staff cannot chart in designated areas:
Patient documentation becomes fragmented and delayed
Communication breakdowns increase patient safety risks
Infection control protocols are compromised (charting in non-clinical spaces)
Staff stress and burnout accelerate
Patient satisfaction declines (staff unavailable for rounds)
This is preventable through proper procurement and governance.
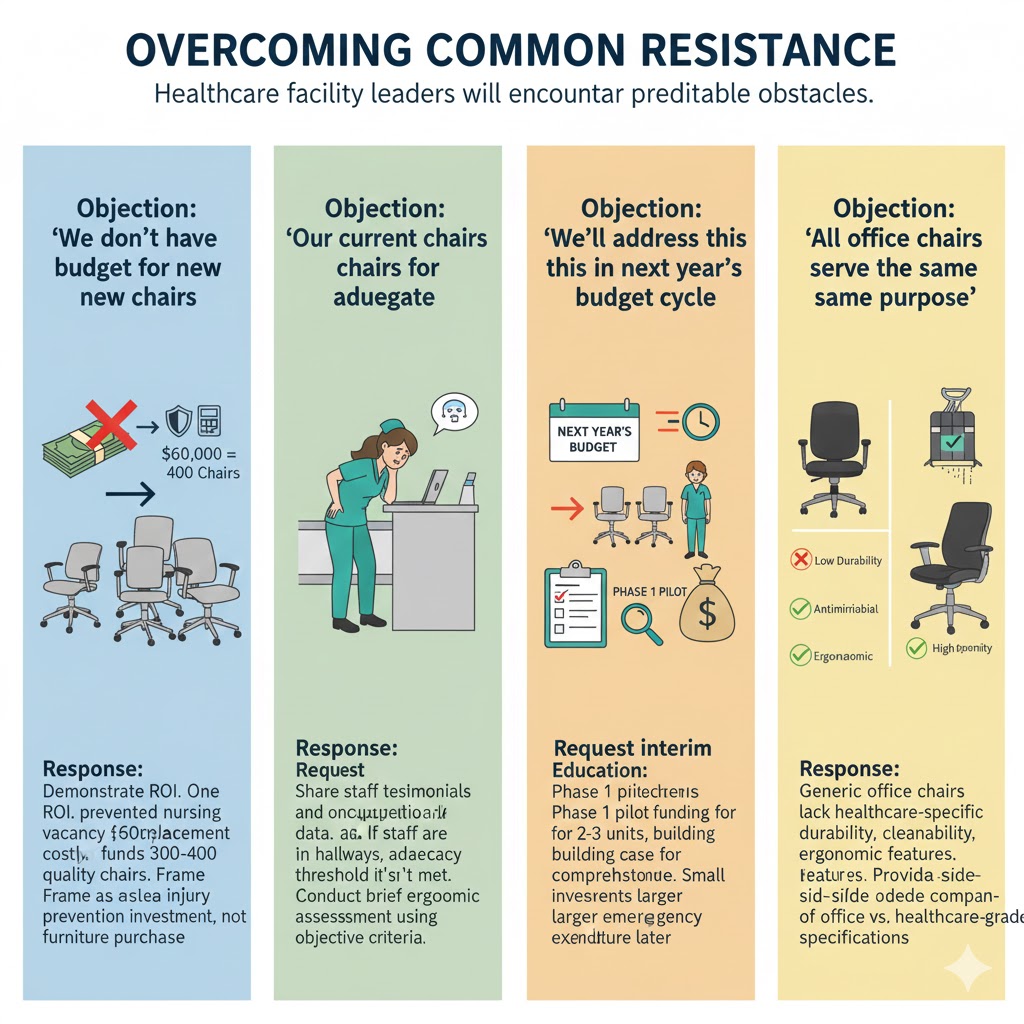
Healthcare facility leaders will encounter predictable obstacles:
Response: Demonstrate ROI. One prevented nursing vacancy ($60,000 replacement cost) funds 300-400 quality chairs. Frame as injury prevention investment, not furniture purchase.
Response: Share staff testimonials and occupational health data. If staff are charting in hallways, adequacy threshold isn't met. Conduct brief ergonomic assessment using objective criteria.
Response: Request interim solutions. Phase 1 pilot funding for 2-3 units demonstrates value, building case for comprehensive funding. Small investment now prevents larger emergency expenditure later.
Response: Education. Generic office chairs lack healthcare-specific durability, cleanability, and ergonomic features. Provide side-by-side comparison of office vs. healthcare-grade specifications.
Healthcare workers operate in physically and emotionally demanding environments. Yet one of the simplest tools supporting their work—a proper, available chair—remains chronically neglected.
This isn't a comfort issue. It's a workplace safety issue, operational efficiency issue, and organizational integrity issue.
When administrators fail to provide basic working conditions, they implicitly communicate that worker well-being ranks below budgetary convenience. Staff respond through turnover, reduced discretionary effort, and compromised care quality.
The solution is straightforward: Implement the four-pillar approach outlined above—establish standards, transform governance, partner with specialized manufacturers, and execute systematic procurement.
Healthcare facilities that take staff seating seriously will experience:
Reduced occupational injuries and workers' compensation claims
Improved staff retention and recruitment
Enhanced patient safety through better staff workflow
Compliance with regulatory standards
Measurable cultural shift prioritizing worker dignity
The next step is yours: Schedule the leadership conversation, authorize the facility audit, and commit to eliminating the corridor charting crisis. Your frontline staff—and ultimately your patients—will benefit from this fundamental investment in working conditions.